Items filtered by date: May 2024
Plantar Fasciitis Is a Degenerative Foot Condition
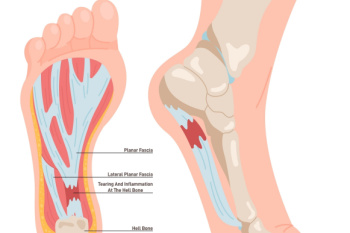
Plantar fasciitis is a foot condition characterized by inflammation and degeneration of the plantar fascia, a thick band of tissue that runs along the bottom of the foot, connecting the heel to the toes. This condition often develops gradually over time, resulting from repetitive strain and stress on the plantar fascia. Activities that involve prolonged standing, walking, or running, especially on hard surfaces, can worsen the problem. Additionally, factors such as obesity, tight calf muscles, high arches, flat feet, and non-supportive footwear can increase the risk of developing plantar fasciitis. Symptoms include heel pain, particularly in the morning or after periods of inactivity, which can worsen with activity. While plantar fasciitis can be challenging to manage, various treatment options, including rest, stretching exercises, orthotic devices, and in severe cases, corticosteroid injections or surgery, can help alleviate pain and promote healing. If you have persistent heel pain, it is strongly suggested that you consult a podiatrist who can accurately diagnose and treat the cause.
Plantar fasciitis is a common foot condition that is often caused by a strain injury. If you are experiencing heel pain or symptoms of plantar fasciitis, contact Leonora Fihman, DPM from California. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is one of the most common causes of heel pain. The plantar fascia is a ligament that connects your heel to the front of your foot. When this ligament becomes inflamed, plantar fasciitis is the result. If you have plantar fasciitis you will have a stabbing pain that usually occurs with your first steps in the morning. As the day progresses and you walk around more, this pain will start to disappear, but it will return after long periods of standing or sitting.
What Causes Plantar Fasciitis?
- Excessive running
- Having high arches in your feet
- Other foot issues such as flat feet
- Pregnancy (due to the sudden weight gain)
- Being on your feet very often
There are some risk factors that may make you more likely to develop plantar fasciitis compared to others. The condition most commonly affects adults between the ages of 40 and 60. It also tends to affect people who are obese because the extra pounds result in extra stress being placed on the plantar fascia.
Prevention
- Take good care of your feet – Wear shoes that have good arch support and heel cushioning.
- Maintain a healthy weight
- If you are a runner, alternate running with other sports that won’t cause heel pain
There are a variety of treatment options available for plantar fasciitis along with the pain that accompanies it. Additionally, physical therapy is a very important component in the treatment process. It is important that you meet with your podiatrist to determine which treatment option is best for you.
If you have any questions, please feel free to contact our offices located in Encino and Brentwood, Los Angeles, CA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Plantar Fasciitis Is a Degenerative Foot Condition
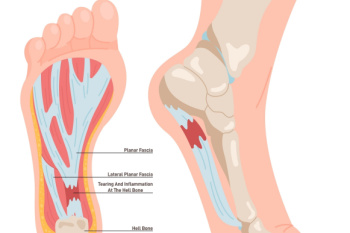
Plantar fasciitis is a foot condition characterized by inflammation and degeneration of the plantar fascia, a thick band of tissue that runs along the bottom of the foot, connecting the heel to the toes. This condition often develops gradually over time, resulting from repetitive strain and stress on the plantar fascia. Activities that involve prolonged standing, walking, or running, especially on hard surfaces, can worsen the problem. Additionally, factors such as obesity, tight calf muscles, high arches, flat feet, and non-supportive footwear can increase the risk of developing plantar fasciitis. Symptoms include heel pain, particularly in the morning or after periods of inactivity, which can worsen with activity. While plantar fasciitis can be challenging to manage, various treatment options, including rest, stretching exercises, orthotic devices, and in severe cases, corticosteroid injections or surgery, can help alleviate pain and promote healing. If you have persistent heel pain, it is strongly suggested that you consult a podiatrist who can accurately diagnose and treat the cause.
Plantar fasciitis is a common foot condition that is often caused by a strain injury. If you are experiencing heel pain or symptoms of plantar fasciitis, contact Leonora Fihman, DPM from California. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is one of the most common causes of heel pain. The plantar fascia is a ligament that connects your heel to the front of your foot. When this ligament becomes inflamed, plantar fasciitis is the result. If you have plantar fasciitis you will have a stabbing pain that usually occurs with your first steps in the morning. As the day progresses and you walk around more, this pain will start to disappear, but it will return after long periods of standing or sitting.
What Causes Plantar Fasciitis?
- Excessive running
- Having high arches in your feet
- Other foot issues such as flat feet
- Pregnancy (due to the sudden weight gain)
- Being on your feet very often
There are some risk factors that may make you more likely to develop plantar fasciitis compared to others. The condition most commonly affects adults between the ages of 40 and 60. It also tends to affect people who are obese because the extra pounds result in extra stress being placed on the plantar fascia.
Prevention
- Take good care of your feet – Wear shoes that have good arch support and heel cushioning.
- Maintain a healthy weight
- If you are a runner, alternate running with other sports that won’t cause heel pain
There are a variety of treatment options available for plantar fasciitis along with the pain that accompanies it. Additionally, physical therapy is a very important component in the treatment process. It is important that you meet with your podiatrist to determine which treatment option is best for you.
If you have any questions, please feel free to contact our offices located in Encino and Brentwood, Los Angeles, CA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Rheumatoid Arthritis and Foot Health

Rheumatoid arthritis, or RA, is a chronic autoimmune condition that can affect various joints throughout the body, including those in the feet and ankles. In RA, the joints become inflamed, leading to pain, swelling, stiffness, and loss of function. Several foot and ankle joints commonly affected by RA include the metatarsophalangeal, or MTP joints, which connect the toes to the foot bones, as well as the subtalar and ankle joints. Inflammation in these joints can cause deformities, such as bunions, hammertoes, and flat feet, that make walking and standing difficult. Additionally, RA can lead to the formation of rheumatoid nodules, which are firm lumps that develop under the skin, often surrounding the Achilles tendon or on the toes. Prompt diagnosis and treatment are essential for managing RA symptoms and preventing joint damage. If you are experiencing stiffness in your feet or ankles, it is suggested that you schedule an appointment with a podiatrist who can suggest treatment options.
Because RA affects more than just your joints, including the joints in your feet and ankles, it is important to seek early diagnosis from your podiatrist if you feel like the pain in your feet might be caused by RA. For more information, contact Leonora Fihman, DPM of California. Our doctor will assist you with all of your podiatric concerns.
What Is Rheumatoid Arthritis?
Rheumatoid Arthritis (RA) is an autoimmune disorder in which the body’s own immune system attacks the membranes surrounding the joints. Inflammation of the lining and eventually the destruction of the joint’s cartilage and bone occur, causing severe pain and immobility.
Rheumatoid Arthritis of the Feet
Although RA usually attacks multiple bones and joints throughout the entire body, almost 90 percent of cases result in pain in the foot or ankle area.
Symptoms
- Swelling and pain in the feet
- Stiffness in the feet
- Pain on the ball or sole of feet
- Joint shift and deformation
Diagnosis
Quick diagnosis of RA in the feet is important so that the podiatrist can treat the area effectively. Your doctor will ask you about your medical history, occupation, and lifestyle to determine the origin of the condition. Rheumatoid Factor tests help to determine if someone is affected by the disease.
If you have any questions please feel free to contact our offices located in Encino and Brentwood, Los Angeles, CA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Rheumatoid Arthritis and Foot Health

Rheumatoid arthritis, or RA, is a chronic autoimmune condition that can affect various joints throughout the body, including those in the feet and ankles. In RA, the joints become inflamed, leading to pain, swelling, stiffness, and loss of function. Several foot and ankle joints commonly affected by RA include the metatarsophalangeal, or MTP joints, which connect the toes to the foot bones, as well as the subtalar and ankle joints. Inflammation in these joints can cause deformities, such as bunions, hammertoes, and flat feet, that make walking and standing difficult. Additionally, RA can lead to the formation of rheumatoid nodules, which are firm lumps that develop under the skin, often surrounding the Achilles tendon or on the toes. Prompt diagnosis and treatment are essential for managing RA symptoms and preventing joint damage. If you are experiencing stiffness in your feet or ankles, it is suggested that you schedule an appointment with a podiatrist who can suggest treatment options.
Because RA affects more than just your joints, including the joints in your feet and ankles, it is important to seek early diagnosis from your podiatrist if you feel like the pain in your feet might be caused by RA. For more information, contact Leonora Fihman, DPM of California. Our doctor will assist you with all of your podiatric concerns.
What Is Rheumatoid Arthritis?
Rheumatoid Arthritis (RA) is an autoimmune disorder in which the body’s own immune system attacks the membranes surrounding the joints. Inflammation of the lining and eventually the destruction of the joint’s cartilage and bone occur, causing severe pain and immobility.
Rheumatoid Arthritis of the Feet
Although RA usually attacks multiple bones and joints throughout the entire body, almost 90 percent of cases result in pain in the foot or ankle area.
Symptoms
- Swelling and pain in the feet
- Stiffness in the feet
- Pain on the ball or sole of feet
- Joint shift and deformation
Diagnosis
Quick diagnosis of RA in the feet is important so that the podiatrist can treat the area effectively. Your doctor will ask you about your medical history, occupation, and lifestyle to determine the origin of the condition. Rheumatoid Factor tests help to determine if someone is affected by the disease.
If you have any questions please feel free to contact our offices located in Encino and Brentwood, Los Angeles, CA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
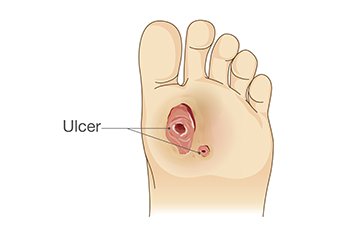
What Is a Diabetic Foot Ulcer?
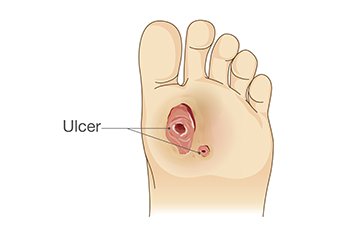 Diabetic foot ulcers are a common and serious complication of diabetes. Ulcers are open sores or wounds that typically appear on the bottom of the foot. They often start as small blisters or cuts but can evolve into deeper wounds due to poor circulation and nerve damage in the feet. This nerve damage, also known as neuropathy, is common in people with diabetes. Neuropathy diminishes the ability to feel pain, allowing injuries to go unnoticed and untreated. Poor blood circulation also reduces the ability of the body to heal, making even minor wounds potentially serious. A diabetic foot ulcer looks like a red crater in the skin, which may weep fluid. The area around the ulcer may be swollen, red, and warm to the touch. Prompt treatment is important to prevent infection and further serious complications, such as gangrene or amputation. Regular foot inspections, maintaining blood sugar levels, and appropriate footwear are key preventative measures for those with diabetes to minimize the risk of developing ulcers. If you have foot ulcers due to diabetes, it is suggested that you consult a podiatrist for regular check-ups.
Diabetic foot ulcers are a common and serious complication of diabetes. Ulcers are open sores or wounds that typically appear on the bottom of the foot. They often start as small blisters or cuts but can evolve into deeper wounds due to poor circulation and nerve damage in the feet. This nerve damage, also known as neuropathy, is common in people with diabetes. Neuropathy diminishes the ability to feel pain, allowing injuries to go unnoticed and untreated. Poor blood circulation also reduces the ability of the body to heal, making even minor wounds potentially serious. A diabetic foot ulcer looks like a red crater in the skin, which may weep fluid. The area around the ulcer may be swollen, red, and warm to the touch. Prompt treatment is important to prevent infection and further serious complications, such as gangrene or amputation. Regular foot inspections, maintaining blood sugar levels, and appropriate footwear are key preventative measures for those with diabetes to minimize the risk of developing ulcers. If you have foot ulcers due to diabetes, it is suggested that you consult a podiatrist for regular check-ups.
Diabetic foot care is important in preventing foot ailments such as ulcers. If you are suffering from diabetes or have any other concerns about your feet, contact Leonora Fihman, DPM from California. Our doctor can provide the care you need to keep you pain-free and on your feet.
Diabetic Foot Care
Diabetes affects millions of people every year. The condition can damage blood vessels in many parts of the body, especially the feet. Because of this, taking care of your feet is essential if you have diabetes, and having a podiatrist help monitor your foot health is highly recommended.
The Importance of Caring for Your Feet
- Routinely inspect your feet for bruises or sores.
- Wear socks that fit your feet comfortably.
- Wear comfortable shoes that provide adequate support.
Patients with diabetes should have their doctor monitor their blood levels, as blood sugar levels play such a huge role in diabetic care. Monitoring these levels on a regular basis is highly advised.
It is always best to inform your healthcare professional of any concerns you may have regarding your feet, especially for diabetic patients. Early treatment and routine foot examinations are keys to maintaining proper health, especially because severe complications can arise if proper treatment is not applied.
If you have any questions please feel free to contact our offices located in Encino and Brentwood, Los Angeles, CA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
What Is a Diabetic Foot Ulcer?
 Diabetic foot ulcers are a common and serious complication of diabetes. Ulcers are open sores or wounds that typically appear on the bottom of the foot. They often start as small blisters or cuts but can evolve into deeper wounds due to poor circulation and nerve damage in the feet. This nerve damage, also known as neuropathy, is common in people with diabetes. Neuropathy diminishes the ability to feel pain, allowing injuries to go unnoticed and untreated. Poor blood circulation also reduces the ability of the body to heal, making even minor wounds potentially serious. A diabetic foot ulcer looks like a red crater in the skin, which may weep fluid. The area around the ulcer may be swollen, red, and warm to the touch. Prompt treatment is important to prevent infection and further serious complications, such as gangrene or amputation. Regular foot inspections, maintaining blood sugar levels, and appropriate footwear are key preventative measures for those with diabetes to minimize the risk of developing ulcers. If you have foot ulcers due to diabetes, it is suggested that you consult a podiatrist for regular check-ups.
Diabetic foot ulcers are a common and serious complication of diabetes. Ulcers are open sores or wounds that typically appear on the bottom of the foot. They often start as small blisters or cuts but can evolve into deeper wounds due to poor circulation and nerve damage in the feet. This nerve damage, also known as neuropathy, is common in people with diabetes. Neuropathy diminishes the ability to feel pain, allowing injuries to go unnoticed and untreated. Poor blood circulation also reduces the ability of the body to heal, making even minor wounds potentially serious. A diabetic foot ulcer looks like a red crater in the skin, which may weep fluid. The area around the ulcer may be swollen, red, and warm to the touch. Prompt treatment is important to prevent infection and further serious complications, such as gangrene or amputation. Regular foot inspections, maintaining blood sugar levels, and appropriate footwear are key preventative measures for those with diabetes to minimize the risk of developing ulcers. If you have foot ulcers due to diabetes, it is suggested that you consult a podiatrist for regular check-ups.
Diabetic foot care is important in preventing foot ailments such as ulcers. If you are suffering from diabetes or have any other concerns about your feet, contact Leonora Fihman, DPM from California. Our doctor can provide the care you need to keep you pain-free and on your feet.
Diabetic Foot Care
Diabetes affects millions of people every year. The condition can damage blood vessels in many parts of the body, especially the feet. Because of this, taking care of your feet is essential if you have diabetes, and having a podiatrist help monitor your foot health is highly recommended.
The Importance of Caring for Your Feet
- Routinely inspect your feet for bruises or sores.
- Wear socks that fit your feet comfortably.
- Wear comfortable shoes that provide adequate support.
Patients with diabetes should have their doctor monitor their blood levels, as blood sugar levels play such a huge role in diabetic care. Monitoring these levels on a regular basis is highly advised.
It is always best to inform your healthcare professional of any concerns you may have regarding your feet, especially for diabetic patients. Early treatment and routine foot examinations are keys to maintaining proper health, especially because severe complications can arise if proper treatment is not applied.
If you have any questions please feel free to contact our offices located in Encino and Brentwood, Los Angeles, CA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Wearing Proper Footwear in Healthcare Work Environments

Wearing appropriate footwear in healthcare settings holds immense importance, impacting the well-being of healthcare professionals and the quality of patient care. Healthcare environments are dynamic and demanding, requiring individuals to be on their feet for extended periods. Proper footwear provides essential support, stability, and protection against workplace hazards such as spills, sharp objects, and potential exposure to biological hazards. Additionally, wearing quality footwear plays an essential role in preventing foot fatigue, discomfort, and musculoskeletal injuries commonly associated with prolonged standing or walking. Furthermore, wearing closed-toe shoes with slip-resistant soles reduces the risk of slips, trips, and falls, promoting a safer working environment for staff and patients. By prioritizing the selection of appropriate footwear, healthcare professionals can enhance their comfort, productivity, and overall well-being, ensuring they can focus on delivering optimal care to those in need while minimizing the risk of workplace-related injuries. If you have foot pain while working, contact a podiatrist who can treat foot conditions and guide you toward the right shoe choices for your working day.
While working on the feet, it is important to take the proper care of them. For more information about working on your feet, contact Leonora Fihman, DPM from California. Our doctor will treat your foot and ankle needs.
Working on Your Feet
Standing on your feet for long periods of time can cause stress and pain in your feet. Your whole body may experience change in terms of posture, back pain, bunions, callouses and or plantar warts. There are ways to avoid these conditions with proper foot care, smart choices and correct posture.
Positive Changes
Negative heeled shoe – Choosing this shoe type places the heel slightly lower than the ball of the foot. These are great for overall foot health. Find shoes that fit you correctly.
Go barefoot – Our feet were not designed to be enclosed for all hours of the day. Try to periodically expose your feet to air.
Eliminate Pain
Foot Exercises – Performing simple exercises, incorporating yoga and doing stretches are beneficial. This will allow increased blood flow to the area and muscles of the foot.
Achilles tendon – Stretching the foot out flat on the floor will relax the calf muscles and tendon. These exercises can be performed almost anywhere. Make sure you add these exercises to your daily regimen.
With a little bit of this information and knowing more about foot health, you will notice changes. Foot stretches and proper footwear will help with pain and prevent further issues.
If you have any questions please feel free to contact our offices located in Encino and Brentwood, Los Angeles, CA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.